Billing and Collections Review Audit Work Program (Healthcare)
Patient Accounts in Focus: An In-Depth Review of Billing and Collection Procedures in Healthcare
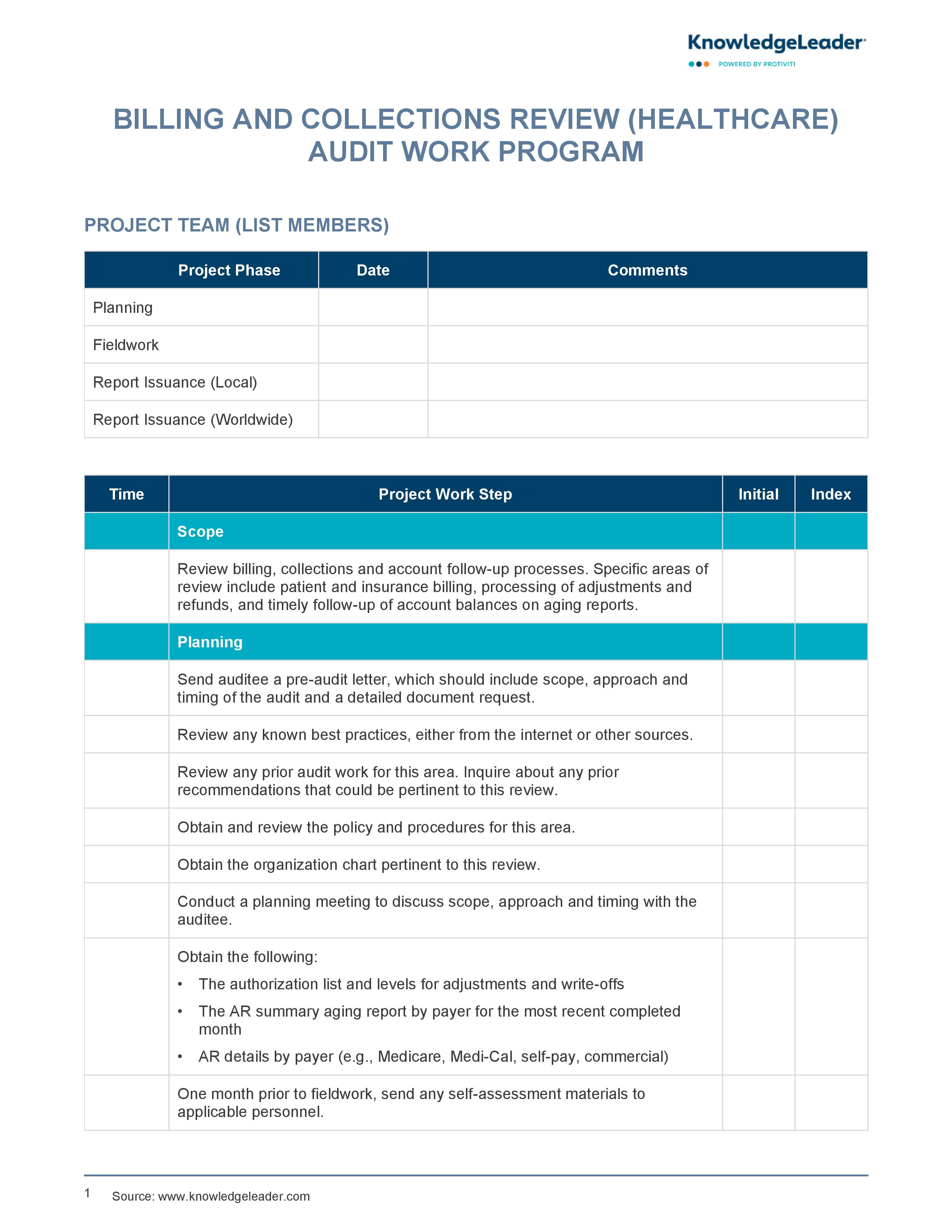
This Billing and Collections Review Audit Work Program provides healthcare organizations with a rigorous framework for assessing their entire revenue cycle, from initial patient intake to final payment. The program guides audit teams through every phase of the engagement, including planning, fieldwork and the issuance of final reports. Its scope is intentionally broad, covering patient and insurance billing, the processing of adjustments and refunds, and the timely follow-up of account balances on aging reports. This tool also ensures that financial operations are scrutinized against both internal policies and industry-best practices by examining payer details across Medicare, Medi-Cal, self-pay and commercial accounts.
Inside, you will find tactical fieldwork procedures, which include detailed sampling methods for testing denied claims, credit balances and bad debt listings, as well as specific steps to evaluate the admission and registration process, ensuring that accurate insurance information is collected at the source to minimize future denials. This tool also assists in verifying critical internal controls, such as the proper segregation of duties in payment posting and the authorization levels for charity write-offs. By using this program to monitor collection agency performance and contract compliance, your team can effectively identify underpayments and maintain a high standard of accuracy throughout the billing process.
Key audit steps include:
- Review any known best practices, either from the internet or other sources.
- One month prior to fieldwork, send any self-assessment materials to applicable personnel.
- Gain an understanding of procedures for account processing (charges, payments, adjustments, contractual allowances, etc.).
- Provide customer satisfaction forms and discuss expectations.